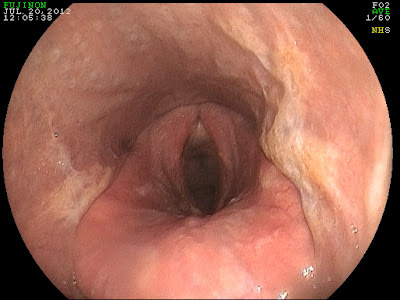
The image above was from a 10 year old gelding that presented for a history of coughing and mild nasal discharge. The cough was intermittent and would vary from day to day. Recently, the cough had worsened as had the summer heat! Based on the history, the most likely cause was predicted to be heaves (AKA: COPD). However, when the endoscope was introduced into the gelding's upper airway it was clear that we were dealing with something quite different. There was evidence of pharyngeal scarring (cicatrix) and active pharyngeal ulceration in a 360 degree (red circle below) range. These findings were consistent with active inflammation and chronic changes. In addition, there was chronic, active inflammation of the arytenoids (green arrow).

The cause of pharyngeal inflammation/ulceration varies and is often never determined. In some cases, it may be complicated by bacterial infection. In some cases, the inciting cause is presumed to be an environmental irritant that the horse is chronically exposed to. The chronic inflammation results in scarring or cicatrix formation that can result in narrowing of the pharynx. Pharyngeal cicatrix formation is a serious complication that has no reliable remedy! As such, a chronic couch (>2 weeks) should be evaluated via endoscopy prior to the development of scarring. Pharyngeal inflammation is typically treated with forced rest and topical antibiotics/steroids in the form of a nasal flush.


















